Seven problems — one laser solution
|
The decisive factor for the successful implementation of the laser in your practice — openness to new ways of carrying out standard dental procedures with a laser |
7 MOST IMPORTANT PROCEDURES FOR THE DEVELOPMENT OF YOUR WATERLASE
|
Doctor GLENN A. VAN AS |
The purchase of the new WaterLase laser is an important event for the practitioner both from a financial point of view and in terms of training. For many people process of learning a new technology can be very difficult; sometimes it is difficult to know where to start. The decisive factor for the successful implementation of the laser in your practice — readiness to learn new techniques and openness to new ways of carrying out standard dental procedures with a laser. Put handpiece MZ5 or MZ6 on tip Gold, turn on the laser in waiting mode, pour water to get everything ready to work — and start learning how to apply the laser to these seven basic procedures. Soon you will start using the laser for other operations.
1. CLASS V RESTORATION
As you age and the process of gum recession due to the use
of drugs and the impact of other factors, root caries is becoming a common
problem
Performing restorations in several quadrants using a WaterLase laser with less
anesthesia, while removing excess (overhanging) soft tissues and caries and
conducting etching enamel with only one application anesthesia, in most cases
becomes
RECOMMENDED SETTINGS FOR CLASS V RESTORATIONS
Ablation of soft tissues: handpiece MZ6: 1,5 W, 50 Hz, water 20 %, air 20
%, mode H (if the tissue is very inflamed, mode S is used).
Ablation of hard tissues: handpiece MZ5: 0,8−2,0 W, 8−15 Hz, 1,5−2,0 W, air
40−60 %, water 60−80 %, mode H.
 |
 |
 |
|
Before intervention |
Immediately after intervention |
Five weeks after the intervention |
 |
2. FRENECTOMY
Frenectomy procedure, which many of us studied while
studying at university, was called
Introduction of lasers into soft tissue surgery opens up new possibilities, as lasers have advantages over traditional methods in that they provide an accurate and clean incision, reduce bleeding, reduce the need for sutures and reduce healing time.
Reduction of postoperative discomfort and faster healing make the use of lasers especially useful in younger patients, as well as in adolescents who need correction of the frenulum simultaneously with orthodontic treatment to close central diastema.
RECOMMENDED SETTINGS FOR FRENECTOMY
Without the use of local anesthetics: handpiece MZ6: 1.5 W, 20 Hz, water
12 %, air 10 %, mode H.
Using local anesthetics: handpiece MZ6: 3.0 W, 40 Hz, water 5 %, air 10 %, mode
H.
Hemostasis (if possible): handpiece MZ6: 0.5 W, 50 Hz, water is turned off, air
10 %, mode S.
 |
 |
 |
| Before intervention |
Immediately after intervention |
Five weeks after the intervention |
3. FIBROMA
Traumatic fibroma (from irritation) occurs most often as a result of the reaction of submucosal tissues to injury by teeth or dentures. This inflammatory hyperplasia is the most common pathological change in the oral cavity, sent for biopsy, and is detected in 1−2 % of adults. It consists of collagen types 1 and 3 and is most often located on the lips, cheek mucosa and lateral sides of the tongue.
Fibromas of the oral cavity are usually asymptomatic, consist of dense tissue and in color do not differ much from healthy tissue if they are not ulcerated due to constant injury. Complaints of patients are often associated with biting fibroma during chewing and dissatisfaction with the appearance if they are located on the lips. With the WaterLase laser, small fibromas can be removed using only application anesthetics, and larger ones — using a few drops of local anesthetic.
Advantages of using laser include reduced bleeding, no
stitches, much shorter duration of intervention and very little discomfort
after the intervention. Minimum penetration depth at the wavelength
RECOMMENDED SETTINGS FOR REMOVAL OF FIBROMAS
Without the use of local anesthetics:
handpiece MZ6: 1.5 W, 20 Hz, water 12 %, air 10 %, mode H.
Using local anesthetics: handpiece MZ6: 3.0 W, 40 Hz, water 5 %, air 10
%, mode H.
Hemostasis (if possible): handpiece MZ6: 0.5 W, 50 Hz, water is turned
off, air 10 %, mode S.
 |
 |
 |
|
Before intervention |
Immediately after intervention |
Two weeks after the intervention |
4. GINGIVECTOMY + SURGICAL CROWN EXTENSION
Gingivectomy is the most common laser procedure on soft
tissues. Removal of excess fixed keratinized tissue, after which there is
enough remaining tissue is necessary for many areas of dentistry. From the
point of view of orthopedics, tissue can prevent the visualization of apical
caries or tubercle fractures below gingival margin. From the point of view of
orthodontics, the tissue
RECOMMENDED SETTINGS FOR GINGIVECTOMY
Without the use of local anesthetics: handpiece MZ5: 1.5 W,
20 Hz, water 20 %, air 20 %, mode H.
Using local anesthetics: handpiece MZ5: 2.1 W, 30 Hz, water 20 %, air 20
%, mode H..
 |
 |
 |
| Before intervention |
During intervention |
Two weeks after the intervention |
5. GINGIVAL RETRACTION
Soft tissue processing for indirect restorations is traditionally carried out using retraction cord to create space for the impression material and to fix the margin position in detail. While digital methods such as intraoral scanners are gaining acceptance, traditional methods are still prevalent. When using both digital and traditional methods of fixing gingival margin, it is difficult to perform manipulations with tissue and work with retraction cord when edge is hidden under the gum. Although we would love to always leave the edge above the gums or at gingival margin level, there are times when a deep edge in the inflamed tissue can be problematic.
Lasers can be used as an additional tool in edge marking and reduce or even eliminate the need for a retraction cord.
Advantages of lasers include hemostasis, less dependence on
hemostatic agents and excellent healing. With WaterLase laser for all tissues,
we can ablate soft tissues as well as small amounts of bone, which can be «on
the way». If left intact, this bone can cause violation of the biological
width, leading to painful, erythematous
RECOMMENDED SETTINGS FOR GINGIVAL RETRACTION
Without the use of local anesthetics:
handpiece MZ5: 1,5 W, 20 Hz, water 12 %, air 10 %, mode H (if the tissue is
very inflamed, mode S is used).
Using local anesthetics: handpiece MZ5: 2.0 W, 50 Hz, water 5 %, air 10 %, mode
H.
Ablation of hard tissues: handpiece MZ5: 4,5 W, 50 Hz, water 90 %, air 60 %,
mode H.
 |
 |
 |
|
Перед вмешательством |
Во время вмешательства |
Через две недели после вмешательства |
6. LASER TREATMENT OF LESIONS OF THE ORAL CAVITY
Today, dentists cured many patients with painful lesions of
the oral cavity, which can complicate the treatment of teeth. With the help of
WaterLase laser it is can to treated lesions such as recurrent aphthous ulcers,
herpetic lesions or decubitalis ulcers from removable dentures. It is important
that the laser can immediately significantly reduce discomfort, but, in
addition, it has been proven that the lesion heals faster due to the effects
RECOMMENDED SETTINGS FOR THE TREATMENT OF LESIONS OF THE ORAL CAVITY
Laser for all tissues WaterLase: handpiece MZ6: 0.25−0.5 W, 50Hz,
water 0 %, air 20 %, mode H.
Diode laser EPIC 10 or iLase: 0.5−0.8 W, CW (constant impulse), new
handpiece, defocusing 2−3 mm.
 |
 |
 |
| Before intervention |
During intervention |
Immediately after intervention |
TREATMENT OF PERIODONTITIS
Traditional treatment of pathological gingival pockets
includes resection technique of partial bone removal, which leads to the fact
that the teeth look like a «breakwater at low tide». The appearance of longer
teeth with healthy pockets often does not satisfy patients who find it harder
to brush their teeth, have to deal with increased tooth sensitivity due to
exposed roots
Regenerative methods to improve the clinical level of
attached gingiva do not give positive results. Many patients are absolutely
amazed to reduce pockets using
REPAIR Protocol can be used for single pathological gingival pockets and generalized periodontitis. It can be used as the first attempt to save implants at initial/moderate bone loss — a problem that is increasingly observed with titanium implants.
|
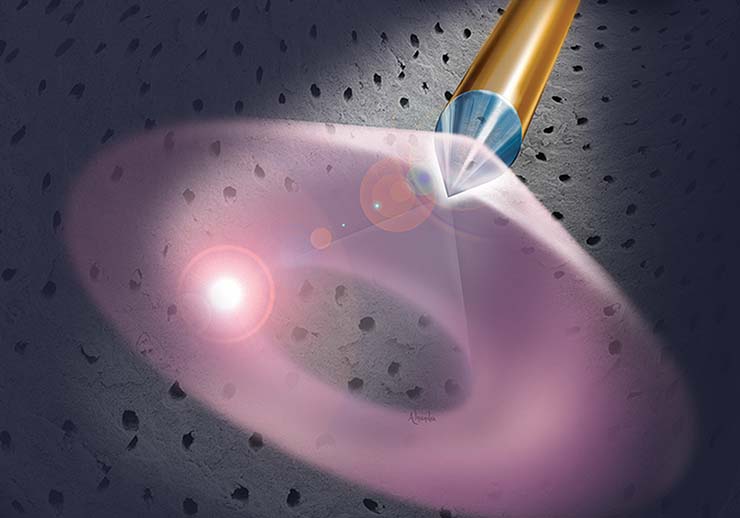
ADDITIONAL PROCEDURE 1: DISINFECTION OF ROOT CANALS Endodontic treatment is necessary in cases where the pulp is inflamed or infected. A common feature of many of these pulp damaging factors is that microorganisms play an important role in the emergence and development of pulp and periapical diseases. Unfortunately, it is not easy to eliminate bacteria. But lasers, unlike other modern devices, have the ability to penetrate deeper into the dentin and provide a tremendous reduction in the number of bacteria without actual direct contact. Thanks to its pulsing high peak power, WaterLase laser provides an incredible photoacoustic flow of stimuli inside root canal, which leads to the removal of bacteria, the opening of dentin tubules and the opening of lateral canals. WaterLase laser with radial handpiece (RFT2 RFT2 and 3), specifically designed for the canals to emit 85% of laser energy laterally and not towards the tip and greatly facilitates cleaning of canals. Laser is used for 60 seconds on each canal after traditional rotary instruments, just before obturation. Microscopic examination of the canals shows incredibly clean surfaces after laser disinfection. RECOMMENDED SETTINGS FOR THE DISINFECTION OF ROOT CANALS Laser cleaning and shaping: handpiece RFT2:
1.25 W, 50Hz, water 10%, air 34 %, mode H. |
|
Introduction
|
PROTOCOL OF TREATMENT OF PERIODONTITIS
Stage 1:
Stage 2: gingivectomy (if necessary).
Stage 3:
Step 4: removal of plaque and root planning.
Step 5: treatment of fissures/degranulation.
Step 6: decortication of bone.
Stage 7: final treatment of fissures.
Stage 8: pressing gauze bandage 2x2.
|
ADDITIONAL PROCEDURE 2: SURGICAL CROWN EXTENSION THROUGH THE BONE In restorative dentistry, clinicians are often faced with the need to reduce small amounts of bone tissue to solve aesthetic or biological problems. In many cases, when tubercle is fractured subcrestally, we would like to «push» the bone apically by 1−2 mm to see if we will restore the tooth, and create an edge that is above the bone. In other cases, we see an opportunity to reduce the asymmetry of soft tissues with a smile, giving the desired shape of a thin bone over the maxillary incisors. This would improve the «pink» aesthetics combined with the «white» aesthetics that our ceramic dentures would provide. In such cases, the laser can be used in the framework of a minimally invasive approach for bone processing by intrafissural (flapless) recontouring. When performing this technique, it is necessary to increase and carefully follow the instructions, but the laser can provide much less postoperative discomfort and reduce the healing time. Laser crown extension can provide perfect healing in two to three weeks, that is, three times faster than the traditional flapped method. The procedure ends with gingivectomy, which provides correction of soft tissues, and restoration of biological width is provided by ablation of hard tissues of the subgingival bone. This procedure can be combined with small flaps at the back to establish the biological width interproximally with just one suture to close the gingival papilla. Laser iPlus, when used for bone remodeling can greatly help in improving aesthetic appearance and function RECOMMENDED SETTINGS FOR RECONTOURING BONE Gingivectomy: handpiece
MZ6: 1.5 W, 30 Hz, water 40 %, air 20 %, mode H.
|
Back














